Why H5 Bird Flu is Not the Next Pandemic
As a retired infectious diseases physician enjoying the fruits of financial independence, I can tell you now that the H5N1 bird flu will not be the next pandemic.
The Current Situation
The UK recently ordered 5 million H5 avian flu vaccine doses as a precautionary measure. In the US, we’ve seen our first severe H5N1 bird flu (which, it seems, was acquired the old-fashioned way from birds rather than cows), with more than 61 reported human cases since April 2024.
Influenza is a known cause of pandemics. It has been done regularly via antigen shift (rather than the drift that causes yearly influenza and yearly changes in the vaccine). It goes from H3 to H1 and causes pandemics. Coronaviruses also cause pandemics (recently in 2020 and before that at least 4 times historically), but when was the last time H5 influenza caused a human pandemic?
When Has H5 Influenza Caused a Pandemic?
H5 influenza has never caused a human pandemic. While H5N1 avian influenza has been a concern for many years, it occasionally infects humans from animals and does not spread effectively between humans.
The first outbreak of human infection by avian influenza H5N1 was observed in 1997 in Hong Kong, resulting in 18 human cases and six deaths. Since then, there have been sporadic human infections due to contact with infected animals.
From 2003 to 2023, the World Health Organization recorded 890 human cases of H5N1 influenza, resulting in 463 deaths worldwide. These cases have not led to sustained human-to-human transmission or a pandemic.
H1 and H3 cause human pandemics. The 2009 H1N1 “swine flu” pandemic was the most recent influenza pandemic. Before that, we had H2 caused by a different influenza A virus subtype.
H2 influenza has caused pandemics in the past. The H2N2 subtype was responsible for the 1957-1958 pandemic, commonly known as the “Asian Flu.” This pandemic emerged in East Asia and spread globally, resulting in an estimated 1.1 million deaths worldwide and 116,000 deaths in the United States.
The H2N2 virus circulated among humans from 1957 to 1968 before being replaced by H3N2.
People born after 1968 lack immunity to H2 viruses, which means many people are susceptible to them (and other non-H1 or H-3 viruses).
Why I’m Not Worried About H5
Limited Human-to-Human Transmission
There is no evidence of the person-to-person spread of H5 bird flu so far. Only H1 and H3 have caused human pandemics.
Exposure Primarily Through Animal Contact
Most human cases of H5N1 have been linked to direct contact with infected birds or cows.
Robust Surveillance and Preparedness
Weird samples are sent to the state and the CDC, where PCR can easily detect the cause of unknown severe infections. mRNA vaccination can be rolled out for the US population within months, so I’m not worried about H5 Bird Flu.
Lessons Learned from COVID-19
The COVID-19 pandemic has taught us valuable lessons about pandemic preparedness. Health systems worldwide are now better equipped to handle potential outbreaks, and we’ve seen improvements in testing capabilities, vaccine development, and public health measures.
Why H5 Bird Flu is Not the Next Pandemic
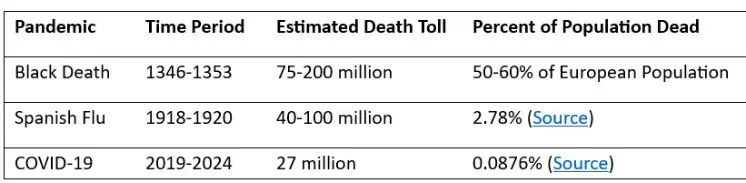
So, why is H5 bird flu unlikely to be the next pandemic? By the way, the last influenza pandemic was in 1918 after a horrible world war. We are in a much better position as a world population to face a pandemic than to emerge from one.
The Nature of the Virus
First, let’s discuss biology. The H5N1 strain of avian influenza primarily affects birds, with chickens, ducks, and turkeys being the most susceptible. The virus has been around since the late 1990s, and while it occasionally infects humans, these instances are rare. Human infections typically occur in close contact with infected birds, not from human-to-human transmission. This is a key point; for a virus to cause a pandemic, efficient human-to-human transmission is essential, something H5N1 has not consistently demonstrated.
Historical Context
Remember the 2004-2005 scare when H5N1 was all over the headlines? We braced for a potential disaster, but it fizzled out. Since then, while sporadic cases have popped up, they haven’t led to sustained outbreaks among humans. The virus hasn’t evolved in a way that would make it more adept at human transmission, and the genetic changes required for such an adaptation haven’t been observed at a concerning rate.
Modern Surveillance and Response
We’re not in the dark ages of public health anymore. Global surveillance systems for influenza are robust. The World Health Organization and other international bodies meticulously track influenza strains. Countries have protocols for culling infected flocks, significantly reducing the risk of spread. Moreover, the lessons from past pandemics have sharpened our response strategies, from vaccine development to public health measures.
Vaccine and Antiviral Readiness
Should H5N1 mutate to become more transmissible among humans, we’re not starting from zero. Vaccines for H5N1 have already been developed, although not in mass production. If needed, these could be ramped up. Additionally, we have antivirals like oseltamivir (Tamiflu) that have shown efficacy against avian flu strains in human cases.
The Misinformation Paradox
In today’s information age, there’s a paradox—we’re flooded with data but also with misinformation. Every new case of H5N1 in humans amplifies the situation, stirring unnecessary panic.
Economic and Agricultural Impact, Not Public Health
H5N1 does significantly impact the poultry industry. Outbreaks can lead to massive culling, affecting the food supply and economies. However, unless the virus mutates significantly, this is an economic rather than a direct public health crisis.
At worst, we cull dairy cow herds.
What We Should Focus On
While H5N1 bird flu is unlikely to cause the next pandemic, it’s still a concern that warrants attention.
Surveillance and R&D are crucial. However, I’m less clear on biosecurity measures such as culling herds and public education, which are always more fraught than the raw milk discussion.
Why H5 Bird Flu is Not the Next Pandemic
I’ve seen my fair share of disease outbreaks as a retired infectious diseases physician. While H5N1 bird flu is certainly a virus we need to monitor, I don’t believe it’s poised to become the next pandemic. The limited human-to-human transmission and improved preparedness and surveillance systems give me confidence that we can handle this threat even though influenza has not jumped this hoop in the history of pandemics.
That said, vigilance is key in the world of infectious diseases. So, while I’m not losing sleep over H5N1, I’ll follow the developments closely—albeit from the comfort of my financially independent retirement!
I’m not saying to ignore H5N1; vigilance is always prudent in infectious diseases. But from my seasoned perspective, the likelihood of sparking the next human pandemic is quite low. Instead of fear, focus on continued surveillance, research, and preparedness. We’re better equipped than ever to handle such threats without succumbing to panic.